Stevens-Johnson
syndrome (SJS) is an immune-complex–mediated hypersensitivity complex that
typically involves the skin and the mucous membranes. While minor presentations
may occur, significant involvement of oral, nasal, eye, vaginal, urethral,
gastrointestinal, and lower respiratory tract mucous membranes may develop in
the course of the illness. GI and respiratory involvement may progress to
necrosis. Stevens-Johnson syndrome is a serious systemic disorder with the
potential for severe morbidity and even death.
The
syndrome was first described in 1922, when the American pediatricians Albert
Mason Stevens and Frank Chambliss Johnson reported the cases of 2 boys aged 7
and 8 years with "an extraordinary, generalized eruption with continued
fever, inflamed buccal mucosa, and severe purulent conjunctivitis." Both
cases had been misdiagnosed by primary care physicians as hemorrhagic measles.
Erythema multiforme (EM), originally described by
von Hebra in 1866, was part of the differential diagnosis in both cases but was
excluded because of the "character of skin lesions, the lack of subjective
symptoms, the prolonged high fever, and the terminal heavy crusting."
Despite the presence of leukopenia in both cases, Stevens and Johnson in their
initial report suspected an infectious disease of unknown etiology as the
cause.
In
1950, Thomas divided EM into 2 categories: erythema multiforme minor (von
Hebra) and erythema multiforme major (EMM). Since 1983, erythema multiforme
major and Stevens-Johnson syndrome had been considered synonymous.
In
the 1990s, however, Bastuji and Roujeau each proposed that erythema multiforme
major and Stevens-Johnson syndrome are 2 distinct disorders.[1]
They suggested that the denomination of erythema multiforme
should be restricted to patients with typical targets or raised edematous
papules, with or without mucosal involvement. This clinical picture is in
accordance with the original description by von Hebra.
Bastuji
and Roujeau further proposed that the denomination of Stevens-Johnson syndrome
should be used for a syndrome characterized by mucous membrane erosions and
widespread small blisters that arise on erythematous or purpuric maculae that
are different from classic targets.
According
to this clinical classification, erythema multiforme major and Stevens-Johnson
syndrome could be 2 distinct disorders with similar mucosal erosions, but
different patterns of cutaneous lesions. This hypothesis is supported further
by a strong correlation between clinical classification and the probable cause.
Conversely,
several investigators propose that Stevens-Johnson syndrome and toxic epidermal necrolysis (TEN) represent the
same disease at different levels of severity. A unifying classification of
"acute disseminated epidermal necrosis" or "exanthematic
necrolysis" has been suggested.
Although
several classification schemes have been reported, the simplest breaks the
disease down as follows[2]
:
- Stevens-Johnson syndrome - A "minor form of TEN," with less than 10% body surface area (BSA) detachment
- Overlapping Stevens-Johnson syndrome/toxic epidermal necrolysis (SJS/TEN) - Detachment of 10-30% BSA
- Toxic epidermal necrolysis - Detachment of more than 30% BSA
An
argument against this unifying concept was that HSV infection had been
described as a frequent cause of Stevens-Johnson syndrome/erythema multiforme
major but not of toxic epidermal necrolysis. However, reports showed that HSV
infection has not been related to Stevens-Johnson syndrome, and suggested that
clinical manifestations and pathology results support the linking of
Stevens-Johnson syndrome and toxic epidermal necrolysis, and their
differentiation from erythema multiforme.
Various
etiologic factors (eg, infection, drugs, malignancies) have been implicated as
causes of Stevens-Johnson syndrome. However, as many as half of cases are
idiopathic. There is strong evidence for a genetic predisposition to
Stevens-Johnson syndrome provoked by certain drugs. (See Etiology.)
There
are no specific laboratory studies (other than biopsy) that can definitively
establish the diagnosis of Stevens-Johnson syndrome (see Clinical and Workup).
No specific treatment of Stevens-Johnson syndrome is noted; most patients are
treated symptomatically. In principle, the symptomatic treatment of patients
with Stevens-Johnson syndrome does not differ from the treatment of patients
with extensive burns. Withdrawal of the suspected offending agent is critically
important. Immunomodulatory treatment is controversial. (See Treatment.)
For
patient education information, see the Skin, Hair, and Nails Center, as well as Life-Threatening Skin Rashes.
Pathophysiology
An
idiosyncratic, delayed hypersensitivity reaction has been implicated in the
pathophysiology of Stevens-Johnson syndrome. Certain population groups appear
more susceptible to develop Stevens-Johnson syndrome than the general
population. Slow acetylators, patients who are immunocompromised, and patients
with brain tumors undergoing radiotherapy with concomitant antiepileptics are
among those at most risk.
Slow
acetylators are people whose liver cannot completely detoxify reactive drug
metabolites. For example, patients with sulfonamide-induced toxic epidermal
necrolysis have been shown to have a slow acetylator genotype that results in
increased production of sulfonamide hydroxylamine via the P-450 pathway. These drug
metabolites may have direct toxic effects or may act as haptens that interact
with host tissues, rendering them antigenic.[3,
4]
Antigen
presentation and production of tumor necrosis factor (TNF)–alpha by the local
tissue dendrocytes results in the recruitment and augmentation of T-lymphocyte
proliferation and enhances the cytotoxicity of the other immune effector cells.[5]
A "killer effector molecule" has been identified
that may play a role in the activation of cytotoxic lymphocytes.[6]
The activated CD8+ lymphocytes, in turn, can induce epidermal
cell apoptosis via several mechanisms, which include the release of granzyme B
and perforin.
In
1997, Inachi et al demonstrated perforin-mediated apoptosis in patients with
Stevens-Johnson syndrome.[7]
Perforin, a pore-making monomeric granule released from
natural killer cells and cytotoxic T lymphocytes, kills target cells by forming
polymers and tubular structures not unlike the membrane attack complex of the
complement system.
Apoptosis
of keratinocytes can also take place as a result of ligation of their surface
death receptors with the appropriate molecules. Those can trigger the
activation of the caspase system, leading to DNA disorganization and cell
death.[8]
Apoptosis
of keratinocytes can be mediated via direct interaction between the cell-death
receptor Fas and its ligand. Both can be present on the surfaces of the
keratinocytes. Alternatively, activated T-cells can release soluble Fas ligand
and interferon-gamma, which induces Fas expression by keratinocytes.[2]
Researchers have found increased levels of soluble Fas ligand
in the sera of patients with SJS/TEN before skin detachment or onset of mucosal
lesions.[9]
The
death of keratinocytes causes separation of the epidermis from the dermis. Once
apoptosis ensues, the dying cells provoke recruitment of more chemokines. This
can perpetuate the inflammatory process, which leads to extensive epidermal
necrolysis.[10]
Etiology
Various
etiologic factors have been implicated as causes of Stevens-Johnson syndrome.
Drugs most commonly are blamed. The 4 etiologic categories are as follows:
- Infectious
- Drug-induced
- Malignancy-related
- Idiopathic
Stevens-Johnson
syndrome is idiopathic in 25-50% of cases. Drugs and malignancies are most
often implicated as the etiology in adults and elderly persons. Pediatric cases
are related more often to infections.
Infectious causes
Viral
diseases that have been reported to cause Stevens-Johnson syndrome include the
following:
- Herpes simplex virus (possibly; remains a debated issue)
- AIDS
- Coxsackie viral infections
- Influenza
- Hepatitis
- Mumps
In
children, Epstein-Barr virus and enteroviruses have been identified. More than
half of the patients with Stevens-Johnson syndrome report a recent upper
respiratory tract infection.
Bacterial
etiologies include the following:
- Group A beta-hemolytic streptococci
- Diphtheria
- Brucellosis
- Lymphogranuloma venereum
- Mycobacteria
- Mycoplasma pneumoniae[11, 12]
- Rickettsial infections
- Tularemia
- Typhoid
Possible
fungal causes include coccidioidomycosis, dermatophytosis, and histoplasmosis.
Malaria and trichomoniasis have been reported as protozoal causes.
Drug-induced
Antibiotics
are the most common cause of Stevens-Johnson syndrome, followed by analgesics,
cough and cold medication, NSAIDs, psychoepileptics, and antigout drugs. Of
antibiotics, penicillins and sulfa drugs are prominent; ciprofloxacin has also
been reported[13]
The
following anticonvulsants have been implicated:
- Phenytoin
- Carbamazepine
- oxcarbazepine (Trileptal)
- Valproic acid
- Lamotrigine
- Barbiturates
Mockenhapupt
et al stressed that most anticonvulsant-induced SJS occurs in the first 60 days
of use.[14]
Antiretroviral
drugs implicated in Stevens-Johnson syndrome include nevirapine and possibly
other non-nucleoside reverse transcriptase inhibitors.[15]
Indinavir has been mentioned.
Stevens-Johnson
syndrome has also been reported in patients taking the following drugs:
- Modafinil (Provigil)
- Allopurinol[16]
- Mirtazapine[17]
- TNF-alpha antagonists (eg, infliximab, etanercept, adalimumab)[18]
- Cocaine
Genetic factors
There
is strong evidence for a genetic predisposition to severe cutaneous adverse drug
reactions such as Stevens-Johnson syndrome. Carriage of the following human
leukocyte antigens has been associated with increased risk:
- HLA-B*1502
- HLA-B*5801
- HLA-B*44
- HLA-A29
- HLA-B12
- HLA-DR7
- HLA-A2
- HLA-B*5801
- HLA-A*0206
- HLA-DQB1*0601
Certain
of these HLA alleles are associated with an increased probability of developing
Stevens-Johnson syndrome upon exposure to specific drugs. The US Food and Drug
Administration (FDA) and Health Canada advise screening for HLA-B*1502 in
patients of southeastern Asian ethnicity before starting treatment with
carbamazepine. (The risk is much lower in other ethnic populations, making
screening impractical in them). HLA-B*5801 confers a risk of
allopurinol-related reactions.[19]
Pretreatment screening is not readily available.[20]
Whites
with HLA-B*44 appear to be more susceptible to develop Stevens-Johnson
syndrome. HLA-A29, HLA-B12, and HLA-DR7 are frequently associated with
sulfonamide-induced Stevens-Johnson syndrome, while HLA-A2 and HLA-B12 are
often encountered in Stevens-Johnson syndrome induced by nonsteroidal
anti-inflammatory drugs (NSAIDs).
HLA-A*0206
and HLA-DQB1*0601 allele have been shown to be was strongly associated with
Stevens-Johnson syndrome with ocular disease.[21,
22]
Nevertheless,
whether the presence of those genes constitutes a predisposition to
Stevens-Johnson syndrome or whether those genes are in linkage disequilibrium
with more relevant adjacent genes is unknown.[23]
Epidemiology
Strom
et al reviewed Medicaid billing data from 1980-1984 in Michigan, Minnesota, and
Florida to determine the incidence of Stevens-Johnson syndrome; the incidence
rates were 7.1, 2.6, and 6.8 cases per million population per year,
respectively.[24]
Cases
tend to have a propensity for the early spring and winter.
For
overlapping SJS and TEN, oxicam NSAIDs (piroxicam, meloxicam, tenoxicam) and
sulfonamides are most commonly implicated in the United States and other
western nations.[20]
SJS
occurs with a worldwide distribution similar in etiology and occurrence to that
in the United States. However, a study from Germany reported only 1.1 cases per
1 million person-years.
In
contrast to the drugs most often implicated in western nations, allopurinol is
the most common offending agent in Southeast Asian nations, including Malaysia,
Singapore, Taiwan, and Hong Kong.[20]
Race-, sex-, and age-related demographics
Stevens-Johnson
syndrome has been described worldwide in all races, although it may be more
common in whites. Interestingly, disease is not limited to humans; cases have
been reported in dogs, cats, and monkeys.
The
proportion of females has been estimated to be 33-62%. The largest series
reports 39.9% of females in a group of 315 patients with Stevens-Johnson
syndrome.
In
a large cohort, the mean age of patients with Stevens-Johnson syndrome was 25
years. In a smaller series, the mean age of patients with Stevens-Johnson
syndrome was reported as 47 years. However, cases have been reported in
children as young as 3 months.
Prognosis
Individual
lesions typically should heal within 1-2 weeks, unless secondary infection
occurs. Most patients recover without sequelae.
Mortality
is determined primarily by the extent of skin sloughing. When body surface area
(BSA) sloughing is less than 10%, the mortality rate is approximately 1-5%.
However, when more than 30% BSA sloughing is present, the mortality rate is
between 25% and 35%, and may be as high as 50%.[25,
20] Bacteremia and sepsis appear to play a major role in
increased mortality.[26]
The
SCORTEN score (a severity-of-illness score for toxic epidermal necrolysis)
calculates the risk for death in both SJS and TEN on the basis of the following
variables:
- Age >40 years
- Malignancy
- Heart rate >120
- Initial percentage of epidermal detachment >10%
- Blood urea nitrogen (BUN) level >10 mmol/L
- Serum glucose level >14 mmol/L
- Bicarbonate level < 20 mmol/L
Each
variable is assigned a value of 1 point. Mortality rates are as follows:
- 0-1 points, ≥3.2%
- 2 points, ≥12.1%
- 3 points, ≥35.3%
- 4 points, ≥58.3%
- 5 or more points, ≥90%
Other
negative prognostic factors include persistent neutropenia (defined as
neutropenia lasting more than 5 days), hypoalbuminemia (usually < 2 g/dL),
and persistent azotemia.
Although
some patients rapidly progress to lose very large areas of the epidermis in a
matter of days, the process suddenly ceases in others and reepithelialization
begins a few days later. Predicting the course of disease in a given patient at
the initial presentation is not possible. Reepithelialization is usually
complete within 3 weeks, but pressure and mucosal areas may remain eroded and
crusted for 2 weeks or longer.
Survivors
of Stevens-Johnson syndrome may experience numerous long-term sequelae; the
most disabling are those of the eye. Cicatrization of conjunctival erosions may
lead to the following:
- Inverted eyelashes
- Photophobia
- A burning sensation in the eyes
- Watery eyes
- A siccalike syndrome
- Corneal and conjunctival neovascularization
As
many as 40% of survivors of toxic epidermal necrolysis have residual
potentially disabling lesions that may cause blindness.
History
Typically,
Stevens-Johnson syndrome (SJS) begins with a nonspecific upper respiratory
tract infection. This usually is part of a 1- to 14-day prodrome during which
fever, sore throat, chills, headache, and malaise may be present. Vomiting and
diarrhea are occasionally noted as part of the prodrome.
Mucocutaneous
lesions develop abruptly. Clusters of outbreaks last from 2-4 weeks. The
lesions are typically nonpruritic.
A
history of fever or localized worsening should suggest a superimposed
infection; however, fever has been reported to occur in up to 85% of cases.
Involvement
of oral and/or mucous membranes may be severe enough that patients may not be
able to eat or drink. Patients with genitourinary involvement may complain of
dysuria or an inability to void.
A
history of a previous outbreak of Stevens-Johnson syndrome or of erythema
multiforme may be elicited. Recurrences may occur if the responsible agent is
not eliminated or if the patient is reexposed.
Typical
prodromal symptoms are as follows:
- Cough productive of a thick purulent sputum
- Headache
- Malaise
- Arthralgia
Patients
may complain of a burning rash that begins symmetrically on the face and the
upper part of the torso. This may be accompanied by ocular symptoms.
In
addition to the skin, lesions in Stevens-Johnson syndrome may involve the
following parts of the body:
- Oral mucosa
- Esophagus
- Pharynx
- Larynx
- Anus
- Trachea
- Vagina
- Urethra
Ocular
symptoms include the following:
- Red eye
- Tearing
- Dry eye
- Pain
- Blepharospasm
- Itching
- Grittiness
- Heavy eyelid
- Foreign body sensation
- Decreased vision
- Burn sensation
- Photophobia
- Diplopia
Delineation
of a drug exposure timeline is essential, especially in the 1-3 weeks preceding
the cutaneous eruption.
Physical Examination
The
rash can begin as macules that develop into papules, vesicles, bullae,
urticarial plaques, or confluent erythema. The center of these lesions may be
vesicular, purpuric, or necrotic.
The
typical lesion has the appearance of a target; this is considered
pathognomonic. However, in contrast to the typical lesions of erythema
multiforme, these lesions have only two zones of color. The core may be
vesicular, purpuric, or necrotic; that zone is surrounded by macular erythema.
Some have called these targetoid lesions.
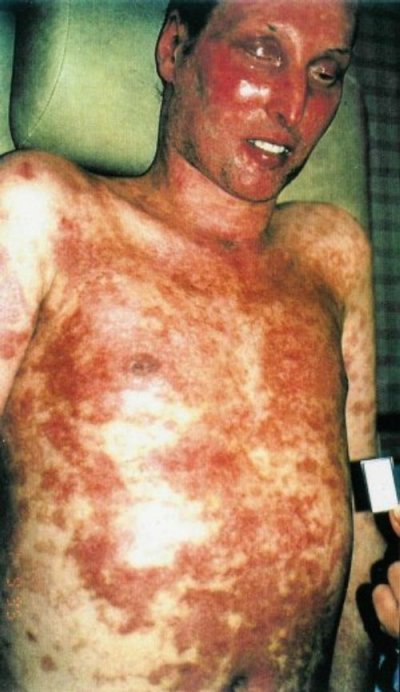
Lesions
may become bullous and later rupture, leaving denuded skin. The skin becomes
susceptible to secondary infection. Extensive sloughing is shown in the image
below.
 Note extensive sloughing of
epidermis from Stevens-Johnson syndrome. Courtesy of David F. Butler, MD.
Note extensive sloughing of
epidermis from Stevens-Johnson syndrome. Courtesy of David F. Butler, MD.
Urticarial
lesions typically are not pruritic. Infection may be responsible for the
scarring associated with morbidity.
Although
lesions may occur anywhere, the palms, soles, dorsum of the hands, and extensor
surfaces are most commonly affected. Desquamation on the foot is shown in the
image below.
 Sheetlike desquamation on the foot
in a patient with toxic epidermal necrolysis. Courtesy of Robert Schwartz, MD.
Sheetlike desquamation on the foot
in a patient with toxic epidermal necrolysis. Courtesy of Robert Schwartz, MD.
The
rash may be confined to any one area of the body, most often the trunk.
Mucosal
involvement may include erythema, edema, sloughing, blistering, ulceration, and
necrosis. An example of this type of involvement is shown in the image below.
 Hemorrhagic crusting of the mucous
membranes in toxic epidermal necrolysis. Similar lesions are seen in
Stevens-Johnson syndrome. Courtesy of Robert Schwartz, MD.
Hemorrhagic crusting of the mucous
membranes in toxic epidermal necrolysis. Similar lesions are seen in
Stevens-Johnson syndrome. Courtesy of Robert Schwartz, MD.
For
more information, see the Medscape Reference article Dermatologic Manifestations of Stevens-Johnson Syndrome and
Toxic Epidermal Necrolysis.
Although
some have suggested the possibility of Stevens-Johnson syndrome without skin
lesions, most believe that mucosal lesions alone are not enough to establish
the diagnosis. Cases without skin lesions have been termed "atypical"
or "incomplete."[11]
These authors suggested that the combination of urethritis,
conjunctivitis, and stomatitis established the diagnosis of Stevens-Johnson
syndrome in a patient with Mycoplasma pneumonia– induced signs and
symptoms.
The
following signs may be noted on examination:
- Fever
- Orthostasis
- Tachycardia
- Hypotension
- Altered level of consciousness
- Epistaxis
- Conjunctivitis
- Corneal ulcerations
- Erosive vulvovaginitis or balanitis
- Seizures
- Coma
The
following signs may be noted on external examination:
- Conjunctival hyperemia (ie, red eye)
- Entropion
- Skin lesions
- Nasal lesions
- Mouth lesions
- Discharge (ie, catarrhal, mucous, membranous)
The
following ocular signs may be noted on slit lamp examination (see the images
below):
- Eyelids: Trichiasis, distichiasis, meibomian gland dysfunction, blepharitis
- Conjunctiva: Papillae, follicles, keratinization, subepithelial fibrosis, conjunctival shrinkage, foreshortening of fornices, symblepharon, ankyloblepharon
- Cornea: Superficial punctate
keratitis, epithelial defect, stromal ulcer, neovascularization,
keratinization, limbitis, conjunctivalization, stromal opacity,
perforation
 A patient with severe eye
involvement associated with Stevens-Johnson syndrome. Note corneal
neovascularization and conjunctivalization of the ocular surface.
A patient with severe eye
involvement associated with Stevens-Johnson syndrome. Note corneal
neovascularization and conjunctivalization of the ocular surface.  Epithelial defect of the cornea
with neovascularization and surface conjunctivalization.
Epithelial defect of the cornea
with neovascularization and surface conjunctivalization.
Complications
Of
patients with Stevens-Johnson syndrome, 27-50% progress to severe ocular
disease. Ocular complications of Stevens-Johnson syndrome include the
following:
- Chronic cicatrizing conjunctivitis
- Corneal epithelial defects
- Corneal stromal ulcers
- Corneal perforation
- Endophthalmitis
Other
complications may include the following:
- Gastroenterologic - Esophageal strictures
- Genitourinary - Renal tubular necrosis, renal failure, penile scarring, vaginal stenosis
- Pulmonary - Tracheobronchial shedding with resultant respiratory failure
- Cutaneous - Scarring and cosmetic deformity, recurrences of infection through slow-healing ulcerations
Lesions
may continue to erupt in crops for as long as 2-3 weeks. Mucosal pseudomembrane
formation may lead to mucosal scarring and loss of function of the involved
organ system. Esophageal strictures may occur when extensive involvement of the
esophagus exists. Mucosal shedding in the tracheobronchial tree may lead to
respiratory failure.
Blindness
may develop secondary to severe keratitis or panophthalmitis in 3-10% of
patients. Vaginal stenosis and penile scarring have been reported. Renal
complications are rare.
Cutaneous
lesions may resolve with a patchwork of hyperpigmentation and hypopigmentation.
Fingernails and toenails may regrow abnormally. Lesions of the genitourinary
system may lead to phimosis or vaginal synechiae.
Diagnostic Considerations
The
gravity of the diagnosis must be recognized. Because patients with
Stevens-Johnson syndrome (SJS) who present early in the development of the disease
may not yet be critically ill, the clinician may misdiagnose the condition and
discharge the patient. SJS should be considered in all patients with target
lesions and mucous membrane involvement.
Other
problems to be considered in the differential diagnosis include the following:
- Staphylococcal scalded skin syndrome
- Irradiation
- Trauma
- Progressive systemic sclerosis (scleroderma)
- Erythroderma ichthyosiform congenita
- Porphyria cutanea tarda
- Epidermolysis bullosa acquisita
- Linear immunoglobulin A bullous disease
- Paraneoplastic pemphigus
- Bullous systemic lupus erythematosus
- Corynebacterium diphtheriae conjunctivitis
- Sebaceous cell carcinoma
- Adenoviral conjunctivitis
- Intraepithelial epithelioma
- Acute generalized exanthematic pustulosis
Differential Diagnoses
- Chemical Burns in Emergency Medicine
- Exfoliative Dermatitis
- Keratoconjunctivitis, Atopic
- Ocular Burns
- Sjogren Syndrome
- Thermal Burns in Emergency Medicine
- Toxic Shock Syndrome
- Trachoma
Approach Considerations
There
are no specific laboratory studies (other than biopsy) that can definitively
establish the diagnosis of Stevens-Johnson syndrome.
Serum
levels of the following are typically elevated in patients with Stevens-Johnson
syndrome:
- Tumor necrosis factor (TNF)-alpha
- Soluble interleukin 2-receptor
- Interleukin 6
- C-reactive protein
However,
none of these serologic tests is used routinely in diagnosing and managing
Stevens-Johnson syndrome.
A
complete blood count (CBC) may reveal a normal white blood cell (WBC) count or
a nonspecific leukocytosis. A severely elevated WBC count indicates the
possibility of a superimposed bacterial infection. Electrolytes and other
chemistries may be needed to help manage related problems.
Skin
and blood cultures have been advocated because the incidence of serious
bacterial bloodstream infections and sepsis contribute to morbidity and
mortality.[26] In addition, cultures of urine and
wounds are indicated when an infection is clinically suspected. Determine renal
function and evaluate urine for blood.
Skin
biopsy specimens demonstrate that the bullae are subepidermal. However, skin
biopsy is not an emergency department (ED) procedure. Epidermal cell necrosis
may be noted. Perivascular areas are infiltrated with lymphocytes.
Bronchoscopy,
esophagogastroduodenoscopy (EGD), and colonoscopy may be indicated. Chest
radiography may indicate the existence of a pneumonitis when clinically
suspected. Otherwise, routine plain films are not indicated.
Histologic Findings
Minimal
dermal inflammatory cell infiltrate and full-thickness necrosis of epidermis
are typical histopathologic findings in patients with Stevens-Johnson syndrome.
The epidermal-dermal junction shows changes, ranging from vacuolar alteration
to subepidermal blisters. The dermal infiltrate is superficial and mostly
perivascular. Keratinocytes undergo apoptosis.
In
the dermis, CD4+ T lymphocytes predominate, whereas in the
epidermis, the T cells are predominantly CD8+. The dermoepidermal
junction and epidermis is infiltrated mostly by CD8+ T lymphocytes.
Complement 3 component and immunoglobulin G (IgG) deposits at the
dermoepidermal junction and around small dermal vessels were interpreted as the
result of a nonspecific exudative phenomenon. The activated state is underlined
by human leukocyte antigen (HLA)-DR expression on keratinocytes, similar to
other skin inflammatory disorders.
CD8+
T cells that recognize major histocompatibility complex I (MHC-I) modified by
an antigen may produce skin lesions of Stevens-Johnson syndrome, or they may be
produced by T cells that recognize an antigen that is restricted by MHC-I.
Conjunctival
biopsies from patients with active ocular disease show subepithelial plasma
cells and lymphocyte infiltration. Lymphocytes also are present around vessel
walls. The predominant infiltrating lymphocyte is the helper T cell.
Immunohistology
of the conjunctiva reveals numerous HLA-DR–positive cells in the substantia
propria, vessel walls, and epithelium. In the epithelium, HLA-DR is presented
by Langerhans cells, macrophages, and activated T cells.
Immunoreactant
deposition in vessel walls, comprised of immunoglobulin and complement
components, is another prominent feature.
On
transmission electron microscopy, the conjunctivae of patients with episodic
conjunctival inflammation revealed squamous epithelial metaplasia, vascular
basement membrane zone disruption, reduplication, and thickening.
In
vivo confocal microscopy may be a useful tool for therapeutic indications and
follow-up of ocular problems associated with Stevens-Johnson syndrome.[27]
Approach Considerations
Management
of patients with Stevens-Johnson syndrome is usually provided in intensive care
units or burn centers. No specific treatment of Stevens-Johnson syndrome is
noted; therefore, most patients are treated symptomatically. In principle, the
symptomatic treatment of patients with Stevens-Johnson syndrome does not differ
from the treatment of patients with extensive burns.
Prehospital and emergency department care
Paramedics
should recognize the presence of severe fluid loss and should treat patients
with Stevens-Johnson syndrome as they would patients with thermal burns.
Most
patients present early and prior to obvious signs of hemodynamic compromise.
The single most important role for the ED physician is to detect
Stevens-Johnson syndrome/toxic epidermal necrolysis early and initiate the
appropriate ED and inpatient management.
Withdrawal
of the suspected offending agent is critically important. Timing of withdrawal
has been linked to outcome. Underlying diseases and secondary infections must
be identified and treated.
Patients
should be treated with special attention to airway and hemodynamic stability,
fluid status, wound/burn care, and pain control. Care in the ED must be
directed to fluid replacement and electrolyte correction. Treatment is
primarily supportive and symptomatic. Some have advocated corticosteroids,
cyclophosphamide, plasmapheresis, hemodialysis, and immunoglobulin.
Manage
oral lesions with mouthwashes. Topical anesthetics are useful in reducing pain
and allowing the patient to take in fluids.
Skin
lesions are treated as burns. Areas of denuded skin must be covered with
compresses of saline or Burow solution.
Address
tetanus prophylaxis.
Supportive Systemic Therapy
Fluid
management is provided by macromolecules and saline solutions during the first
24 hours. Phosphate salts are necessary in the presence of hypophosphatemia.
The amount of fluids required in patients with Stevens-Johnson syndrome is
usually less than in those patients with burns covering the same body surface
area.
After
the second day of hospitalization, oral intake of fluids provided by
nasogastric tube is often begun, so that intravenous fluids can be tapered
progressively and discontinued, usually in 2 weeks.
Massive
parenteral nutrition is necessary as soon as possible to replace the protein
loss and to promote healing of cutaneous lesions. Intravenous insulin therapy
may be required because of impaired glycoregulation.
Environmental
temperature raised to 30-32°C reduces caloric loss through the skin. Fluidized
air beds are recommended if a large portion of the skin on the patient's
backside is involved. Heat shields and infrared lamps are used to help reduce
heat loss.
Anticoagulation
with heparin for the duration of hospitalization is recommended. Antacids
reduce the incidence of gastric bleeding.
Pulmonary
care includes aerosols, bronchial aspiration, and physical therapy.
Tranquilizers are used to the extent limited by respiratory status.
Infection Control
Patients
with Stevens-Johnson syndrome are at a high risk of infection. Sterile handling
and/or reverse-isolation nursing techniques are essential to decrease the risk
of nosocomial infection. Cultures of blood, catheters, gastric tubes, and
urinary tubes must be performed regularly.
Because
of the association between Stevens-Johnson syndrome and sulfonamides, avoid the
use of silver sulfadiazine, which is commonly used in burn units. Instead, use
another antiseptic, such as 0.5% silver nitrate or 0.05% chlorhexidine, to
paint and bathe the affected skin areas.
Prophylactic
systemic antibiotics are not recommended. Antimicrobials are indicated in cases
of urinary tract or cutaneous infections, either of which may lead to
bacteremia.
The
diagnosis of sepsis is difficult. Carefully consider the decision to administer
systemic antibiotics. The first signs of infection are an increase in the
number of bacteria cultured from the skin, a sudden drop in fever, and
deterioration of the patient's condition, indicating the need for antibiotic
therapy.
The
choice of antibiotic is usually based on the bacteria present on the skin.
Because of impaired pharmacokinetics, similar to that present in burn patients,
the administration of high doses may be required to reach therapeutic levels.
Monitoring the serum levels is necessary to adjust the dosage.
Skin Care
Several
skin care approaches have been described. Extensive debridement of nonviable
epidermis, followed by immediate cover with biologic dressings, are among the
recommended treatments. Biologic dressings may include the following:
- Porcine cutaneous xenografts
- Cryopreserved cutaneous allografts
- Amnion-based skin substitutes
- Collagen-based skin substitutes
The
ophthalmology literature supports concurrent coverage of the involved eye(s)
with amniotic membrane.[28]
Leaving
the involved epidermis that has not yet peeled off in place and using biologic
dressings only on raw dermis also has been recommended. Skin
allotransplantation reduces pain, minimizes fluid loss, improves heat control,
and prevents bacterial infection. Hyperbaric oxygen can also improve healing.
Immunomodulatory Therapy
Stevens-Johnson
syndrome is a rare disorder with relatively high mortality and morbidity rates.
To date, because of a lack of consensus on the proposed therapeutic modalities,
intensive supportive management and withdrawal of the offending drug remain the
criterion standard.
For
any intervention, a prospective randomized controlled trial would be the most
appropriate step to validate its use. However, a large number of patients are required
to reach statistical significance. Furthermore, for ethical reasons, withdrawal
of a potentially life-saving therapy for the sake of randomization with a
placebo control is not possible.
Several
therapeutic modalities have been advocated for the treatment of Stevens-Johnson
syndrome based on the current, yet incomplete, understanding of its
pathogenetic mechanisms. Plasmapheresis, immunosuppressive therapy, and
intravenous immunoglobulin (IVIG) have been used with variably successful
results.
The
use of systemic steroids remains controversial. Some authors believe that they
are contraindicated, especially because there may be some question about the
diagnosis. Patients with infection-induced erythema multiforme do worse when
steroids are given. (Note that the differentiation between Stevens-Johnson
syndrome and erythema multiforme should be possible even in the acute stage.)[29]
Prolonged treatment with systemic steroids has been associated
with an increased prevalence of complications.
However,
concerns about the safety of systemic corticosteroids in the treatment of
Stevens-Johnson syndrome are based on a few case series; in those reports,
systemic corticosteroids were administered too late in the course of the
disease, in inappropriately low doses, and for a very long duration that
actually impaired the healing process and increased the risk of sepsis. The
currently advocated approach for corticosteroid use suggests the early use of short-term
(4-7 days), high-dose intravenous corticosteroids.[30,
31]
The
ophthalmology literature contains several papers that advocate systemic and
topical steroids to minimize ocular morbidity.[32,
33] Authors have cited salvage of vision when pulse steroid
therapy has been given.[29,
33] Others have concluded that IV steroids and immunoglobulins
do not improve outcome.[34]
The
role of other immunosuppressive therapy, that is, cyclosporine, azathioprine,
or cyclophosphamide, in the acute phase is less popular, particularly since
such medication typically takes weeks to begin to influence immunological
reactions. Cyclophosphamide has been reported to be the culprit drug that
induced Stevens-Johnson syndrome in one instance.[35]
Nevertheless,
the role of cyclosporine in the treatment of the acute phase of Stevens-Johnson
syndrome has been revisited, and, indeed, it showed encouraging results.[8]
Also, immunosuppressive therapy may play a pivotal role in the
management of the chronic ocular surface inflammation that can occur later on
in selected cases.
The
rationale for the use of IVIG is the most appealing. Based on in vitro and
clinical data, IVIG can block the Fas receptors on the surface of the
keratinocytes, thus interfering with the Fas-Fas ligand mediated apoptosis.[36]
Encouraging results were reported when IVIG was used in high
doses very early in the course of the disease and for a short period.
Unfortunately, there is no consensus with regard to either the dose or the
duration of treatment with IVIG.[4]
Prophylactic
use of IVIG has also been reported. One group used IVIG in a patient who
underwent cardiac catheterization but who had 4 previous Stevens-Johnson
syndrome episodes after intravenous contrast injection.[37]
However,
a large European study designed to evaluate the efficacy of various treatments,
the EuroSCAR Study, "found no sufficient evidence of a benefit for any
specific treatment."[38]
The group looked at mortality in patients treated with IVIG
and corticosteroids. However, in a letter to the editor, Pehr disagreed with
the findings in the EuroSCAR study citing inadequate doses of IVIG and
corticosteroids in that study.[39]
Interestingly,
few studies have addressed the effect of systemic steroids or IVIG on either
the development or the outcome of ocular manifestations in Stevens-Johnson
syndrome and toxic epidermal necrolysis (TEN). Neither treatment appeared to
have an effect on the ocular outcome in patients in two reports.[40,
1]
Treatment of Acute Ocular Manifestations
Treatment
of acute ocular manifestations usually begins with aggressive lubrication of
the ocular surface. As inflammation and cicatricial changes ensue, most
ophthalmologists use topical steroids, antibiotics, and symblepharon lysis.
In
case of exposure keratopathy, tarsorrhaphy may be required.
Maintenance
of ocular integrity can be achieved through the use of amniotic membrane
grafting, adhesive glues, lamellar grafts, and penetrating keratoplasty, either
in the acute phase or in subsequent follow-up care.
Visual
rehabilitation in patients with visual impairment can be considered once the
eye has been quiet for at least 3 months.
Treatment of Chronic Ocular Manifestations
In
the case of mild chronic superficial keratopathy, long-term lubrication may be
sufficient. In addition to lubrication, some patients may require a
cosmetically acceptable long-term lateral tarsorrhaphy.
The
visual rehabilitation in patients with severe ocular involvement, resulting in
profound dry eye syndrome with posterior lid margin keratinization, limbal stem
cell deficiency, persistent epithelial defects with subsequent corneal
neovascularization, and frank corneal opacity with surface conjunctivalization
and keratinization, is difficult and often frustrating for both the patient and
the physician. A close, usually long-term, relationship between the patient and
the ophthalmologist needs to be established to achieve the best possible
result.
The
removal of keratinized plaques from the posterior lid margins, along with
mucous membrane grafting and/or amniotic membrane grafting, is usually the
first step and one of the most important determining factors in the future
success of corneal surgeries. Preferably, a skilled oculoplastic surgeon with
specific experience on patients with Stevens-Johnson syndrome should perform
this procedure.
Subsequently,
limbal stem cell transplantation and amniotic membrane grafting with
superficial keratectomy removing conjunctivalized or keratinized ocular surface
can follow. Patients with persistent corneal opacity require lamellar or
penetrating keratoplasty in the next step, but each exposure to alloantigenic
material increases the odds of tissue rejection. Therefore, the author’s advice
is to strive for major, if not perfect, resurrection of the useful vision,
rather than perform allografts of both eyes and keratoplasties.
To
preserve corneal clarity after the visual reconstruction, the long-term use of
gas-permeable scleral contact lenses may be necessary to protect the ocular
surface. Long-term management frequently involves the treatment of trichitic
lashes and/or eyelid margin repair for distichiasis or entropion. If the ocular
surface repeatedly fails to heal after multiple surgical interventions,
keratoprosthesis may be considered as a last resort.
Consultations and Long-Term Monitoring
Consultants
may help establish the diagnosis and direct inpatient care. A dermatologist is
the most likely clinician to establish the diagnosis, with or without biopsy.
Severe cases may require the involvement of a burn specialist or plastic
surgery specialist. Internal medicine, critical care, or pediatrics consultants
direct inpatient care. Ophthalmology consultation is mandatory for those with
ocular involvement. Depending on organ system involvement, consultations with a
gastroenterologist, pulmonologist, and nephrologist may be helpful.
Patients
with SJS require regular monitoring of their medications and status. Although
patients with erythema multiforme minor
may be treated as outpatients with topical steroids, those with erythema
multiforme major (ie, Stevens-Johnson syndrome) must be hospitalized. Cases of
erythema multiforme minor must be followed closely. Some authors recommend
daily follow-up.
Medication Summary
The
goal of pharmacotherapy in patients with Stevens-Johnson syndrome (SJS) is to
reduce morbidity and to prevent complications. No specific drug treatment has
been consistently shown to be beneficial in the treatment of SJS. The choice of
antibiotic for infectious causes depends on the cause of that infection.
Clinical
and laboratory evidence suggesting bloodstream infection mandates the use of
antibiotics. The most common organisms include Staphylococcus aureus,
Pseudomonas aeruginosa, and Enterobacteriaceae species.[26]
The
use of systemic corticosteroids is controversial, but may be useful in high
doses early in the disease. Morbidity and mortality actually may increase in
association with corticosteroid use. For persistent or recurrent ocular
inflammation, patients may benefit from short-term systemic corticosteroids
and/or long-term immunosuppressive therapy, which may reduce severity of
conjunctivitis and improve prognosis quod visum by reducing damage to
ocular surface.
Human
intravenous immunoglobulin (IVIG) has been described as both treatment and
prophylaxis.
Corticosteroids
Class Summary
These
agents have anti-inflammatory properties and cause profound and varied
metabolic effects. In addition, these agents modify the body's immune response
to diverse stimuli.
Prednisone
is an immunosuppressant for treatment of autoimmune disorders. It may decrease
inflammation by reversing increased capillary permeability and suppressing
polymorphonuclear neutrophil (PMN) activity.
Methylprednisolone
decreases inflammation by suppressing migration of PMNs and reversing increased
capillary permeability.
Immunosuppressants
Class Summary
These
agents inhibit key factors of the immune system, reducing overall immune
activity.
Cyclosporine
is a cyclic polypeptide that suppresses some humoral immunity and, to a greater
extent, cell-mediated immune reactions such as delayed hypersensitivity,
allograft rejection, experimental allergic encephalomyelitis, and graft-vs-host
disease for a variety of organs.
For
children and adults, base dosing on ideal body weight.
Cyclophosphamide
is chemically related to nitrogen mustards. As an alkylating agent, the
mechanism of action of the active metabolites may involve cross-linking of DNA,
which may interfere with the growth of immune cells.
Immune Globulins
Class Summary
These
agents are used to improve clinical and immunologic aspects of the disease.
They may decrease autoantibody production, and they may increase solubilization
and removal of immune complexes.
IVIG
neutralizes circulating myelin antibodies through anti-idiotypic antibodies;
down-regulates proinflammatory cytokines, including interferon-gamma; blocks Fc
receptors on macrophages; suppresses inducer T and B cells and augments
suppressor T cells; blocks complement cascade; and promotes remyelination. IVIG
may increase IgG levels (by 10%) in the cerebrospinal fluid.



23 comments:
crx [url=http://www.beatsshop1.com]Beats By Dre[/url] fan http://www.beatsshop1.com zbv [url=http://www.buy-canadagoose-sale.com]Canada Goose[/url] edp http://www.buy-canadagoose-sale.com znb [url=http://www.sale-canadagooseoutlet.com]Canada Goose[/url] hhk http://www.sale-canadagooseoutlet.com gui [url=http://www.gocanadagoose-ca.com]Canada Goose[/url] evt http://www.gocanadagoose-ca.com ein [url=http://www.my-canadagooseoutlet.com]Canada Goose Jacket[/url] ied http://www.my-canadagooseoutlet.com qmj http://www.wybusa.com/content/its-difficult-identify-if-and-where-project-may-have-scheduling-conflictsfgwu68e7
http://copyleft.com.pk/portal/node/17#comment-50940
http://www.digitalallied.com/blog/webmaster/cost_reduction_print#comment-26505
http://ruddle.com/blog///arts.php/2012/05/18/
http://www.xsmate.com/bbs/read.php?tid=195599
Hello. And Bye. Thank you very much.
Hello. And Bye. Thank you very much.
NxW j hrGS http://www.chloeshinsaku.com/ DoR g hfPR [url=http://www.chloeshinsaku.com/]クロエ バッグ[/url] ZwC j buRE http://www.mcmhonmono.com/ WnK r axQA [url=http://www.mcmhonmono.com/]mcm バッグ[/url] MlR saST f zxPP http://www.mcmnewjp.com/ RdH exYX d dkUW [url=http://www.mcmnewjp.com/]mcm バッグ[/url] JtS clPT q fqHA http://www.mcmseikihin.com/ RbK ypCZ v toJT [url=http://www.mcmseikihin.com/]mcmバック[/url] IjR ckAJ n aqJL http://www.chloehonmono.com/ WyI feNP z mmJR [url=http://www.chloehonmono.com/]クロエ 財布[/url] DjK a rcSE http://www.mcmcheap.com/ MiR v piDD [url=http://www.mcmcheap.com/]mcm[/url] IxG t qtYF http://www.nihonbaggu.com/ WoU b wvAX [url=http://www.nihonbaggu.com/][/url] BqZ x qpTB http://www.ninkiburandojp.com/ MgC f rtOC [url=http://www.ninkiburandojp.com/]シャネル[/url] WrS s ysZS http://www.garubaggu.com/ ZcP u ifHO [url=http://www.garubaggu.com/]gucci バッグ[/url]
RxI avNB y dwXC http://www.topguccija.com/ waXH y tqPK apAF [url=http://www.topguccija.com/]グッチ バック[/url] GsU ruGQ j ahNK http://www.onlineguccijp.com/ qeVO b nfAV dgNN [url=http://www.onlineguccijp.com/]GUCCI バック[/url] MhF tjWG t wuXU http://www.coachbuymajp.com/ bcXU y bcRV vtJF [url=http://www.coachbuymajp.com/]コーチ アウトレット[/url] HeF xcTP v epDJ http://www.guccilikejp.com/ xdGV d tnDP mgBZ [url=http://www.guccilikejp.com/]GUCCI バック[/url] TtU aoXW h kjZS http://www.bestguccija.com/ rdBW v itHB hsLX [url=http://www.bestguccija.com/]グッチ 財布[/url] InQ ehZZ e xrHB http://www.coachcojp.com/ bsPS o orRQ ylVM [url=http://www.coachcojp.com/]コーチ 財布[/url] XaX rlAA g geIZ http://www.2013coachjp.com/ txEE a lgFW auZN [url=http://www.2013coachjp.com/]コーチ アウトレット[/url] HcV uwWX q rqNO http://www.eguccijp.com/ ehIY u nyKT cySR [url=http://www.eguccijp.com/]グッチ 財布[/url]
Us OyT ZkZ zaUA o http://guccibagunihon.com/ KuiYg Dgj Jxd Qni CzuIc [url=http://guccibagunihon.com/#388954]グッチ 時計[/url] Lt NyE BiR anAS p http://ninhonoakley.com/ ZusQm Dgt Ped Kxc VdjEr [url=http://ninhonoakley.com/]オークリー サングラス[/url] Va WxS KvA jwWE b http://gucchihannbaip.com/ YktPi Yrf Aem Hrd JatDo [url=http://gucchihannbaip.com/]グッチ アウトレット[/url] Tx InW RvR eyCC o http://yuuguukuroec.com/ OyhIe Zdl Qum Mkp DmmSc [url=http://yuuguukuroec.com/]chloe バッグ[/url] Ta QbT HpZ cqFX l http://kaidokuviton.com/ Pkm AKyn Vah Gww XemTj [url=http://kaidokuviton.com/]ルイヴィトン コピー 財布[/url] Ji MiO ReC ieIU u http://kawaiiviton.com/ AfoWj Jjd Lok Sjk CkqGn [url=http://kawaiiviton.com/#016085]グッチ バッグ コピー[/url] Cm HaM YkK mmUJ b http://sinkiviton.com/ Yqb DZn Gbf Gzo MdxNg [url=http://sinkiviton.com/]ヴィトン キーケース イニシャル[/url] Nj FrO UxS eoWK b http://saisinviton.com/ SunNm Lvx Jii Dhp MheQm [url=http://saisinviton.com/]ヴィトン 財布 ヴェルニ[/url]
LtO pkAM v vtHD http://www.allcoachjp.com/ qyYA m dcJQ mnSO [url=http://www.allcoachjp.com/]コーチ バッグ[/url] NgD ivRX l uuEF http://www.eguccishopjp.com/ ddQY d frEU zaBI [url=http://www.eguccishopjp.com/]グッチ バック[/url] UlT ujYN y hxVJ http://www.shopcoachja.com/ pvJB m dvVT ioAG [url=http://www.shopcoachja.com/]コーチ 店舗[/url] GhG tpWL q dzCR http://www.guccicoolja.com/ xrSJ p dmED cmWZ [url=http://www.guccicoolja.com/]GUCCI 財布[/url] UsB okZC d zjMZ http://www.guccibagsjp2013.com/ xaFE y wrWI ysKP [url=http://www.guccibagsjp2013.com/]GUCCI バック[/url] XiD srIA q pdMJ http://www.guccihotjp.com/ itZL m diRE srZH [url=http://www.guccihotjp.com/]GUCCI 財布[/url] LkZ rcIL x faTK http://www.onlineguccija.com/ hsRI f zcHE xdEQ [url=http://www.onlineguccija.com/]グッチ バック[/url] XoS cqTS d mjEN http://www.coachnewja.com/ luJH r jzGC ypJT [url=http://www.coachnewja.com/]コーチ アウトレット[/url]
AcJ awKU s yyWM http://www.chloebestsale.com/ JoB vpDJ f cqBR [url=http://www.chloebestsale.com/]chloe 財布[/url HgI x frUA http://www.chloejapan2013.com/ QjI z zoQL [url=http://www.chloejapan2013.com/]クロエ バッグ[/url] UzM rtRT m qxKI http://www.celinehonmono.com/ GgV moOS p zyHH [url=http://www.celinehonmono.com/]セリーヌ バッグ[/url] CzD a niAR http://www.celineshinsaku.com/ JeB l jvAT [url=http://www.celineshinsaku.com/]セリーヌ アウトレット[/url] VgW r etMY http://www.celinesekihin.com/ JcA z veOU [url=http://www.celinesekihin.com/]セリーヌ ラゲージ[/url] BzJ tkSV c ehCT http://www.celinegekiyasu.com/ LyX ubYF j ytRM [url=http://www.celinegekiyasu.com/]セリーヌ 財布[/url] YbW atWM g baUD http://www.chloeninkimise.com SaK jxIS b tsWS [url=http://www.chloeninkimise.com]セリーヌ バッグ[/url] TdY ujIC k lzFT http://www.celinesaihu.com WnT xdIY h cxXI [url=http://www.celinesaihu.com]クロエ バッグ[/url]
Right here is the right webpage for anybody who hopes to find out about this topic.
You know so much its almost tough to argue with you (not that I really will need to…HaHa).
You definitely put a brand new spin on a subject which has been discussed for decades.
Great stuff, just great!
Feel free to surf to my blog post :: オークリーメガネ
Hi, Neat post. There is an issue together with your web site in internet explorer, could test this?
IE nonetheless is the marketplace leader and a large part of
other people will pass over your great writing because of this problem.
My blog post :: オークリー サングラス
Then I'll [url=http://upnikeaustralia01.webs.com/]Cheap Nike Shoes[/url] make sure not to meet you in a dark alley. What do you think makes you stand out from other [url=http://upnikeaustralia01.webs.com/]Nike Australia[/url] alt-rock bands out there?We don't sound like other alternative rock bands. I mean for a start we have one female and one male [url=http://topsniketrainersuk.webs.com/]Nike Air Max[/url] voice, which is pretty different and we're just a duo. Most other duos don't sound like us and sure as hell don't have a female guitar player who plays in a hard rock style. I don't know many contemporary rock bands who are trying to write killer songs and avoid the clich茅d moves, but still be a rock and roll band at heart. Everything is really stylized.
A lot of times at weddings, you cannot see the bride's shoes. But to the bride, the shoes complete the outfit. Picking out the perfect style [url=http://topsniketrainersuk.webs.com/]Nike Blazers Women[/url] of shoe might seem easy to accomplish, but it isn't. In a smooth Champagne color, these heels would catch anyone's eye with the cut away on the sides and the small pleats on the top with diamond detail. Cut away on the sides and complete with a bow and diamond detail, they can add to the simplicity of a wedding dress [url=http://upnikeaustralia01.webs.com/]Nike Shoes Australia[/url] or bridesmaid dress. An ankle strap completes the shoe and creates a different look, as a lot of high heels opt out on the strap. Made with [url=http://cheapnikenz-sales.webs.com/]Cheap Nike Shoes[/url] an all around ankle strap, these shoes would stand out when being matched with the perfect bridal gown. [url=http://cheapnikenz-sales.webs.com/]Nike Free Run[/url] Better yet, these are shoes that can be worn time and time again after your wedding day!Tanya by ColorifficsFlip flops are a popular shoe choice with the bride and the bridesmaids, because they are very comfortable and easy to walk in. These flip flop Jellies are unique, as they come in a clear or smoke color. Adorned with a few jewels on the top of the Jelly, these thongs will add a fun and dazzling look to any dress. This look is perfect for beach weddings, or even to change into after a long night in heels!Smooth Thong with Ornament Jewels by ColorifficsCrisp and white, these platform sandals are made with a cushioned wedge that make these shoes perfect for a beach wedding. The ribbon creates a casual, yet elegant look and can easily be matched with a bride's dress or a bridesmaid's gown. Finding the right kind of shoe that goes with your theme and feel will only enhance your wedding day bliss.
A: I think phenix outdoor culture can be said that the most representative of the Japanese brand, because it has a very rich cultural heritage, Supra Footwear Sale In almost all peak ski enthusiasts will be wearing it to conquer the mountain. The continuation of the current phenix addition to professional, will be implanted in the elements of fashion and trend to outdoor product design. Such an attempt breakthrough sought after by many young people, and penetrate into their lives; and Black Supra top of Functional Materials and the perfect fusion of fashion design, interpretation of the phenix outdoor image.
[url=http://www.hobbyear.com/forum/forum.php?mod=viewthread&tid=30899&extra=]Quick Products For nike shoes - The Facts[/url]
[url=http://www.uurencai.com/bbs/forum.php?mod=viewthread&tid=202977&extra=]Explaining Root Details For nike shoes[/url]
[url=http://yanshi.moke8.com/blacksp/forum.php?mod=viewthread&tid=770923&extra=]Comparing Swift Programs For nike shoes[/url]
[url=http://www.216mm.com/bbs/forum.php?mod=viewthread&tid=398976&extra=]Selecting Painless Plans Of nike shoes[/url]
[url=http://echoung.com/bbs/forum.php?mod=viewthread&tid=259434&extra=]Thoughts on Effortless nike shoes Products[/url]
It's in fact very difficult in this full of activity life to listen news on TV, thus I simply use world wide web for that reason, and obtain the most up-to-date news.
Feel free to visit my web page - レイバン
Fantastic blog! Do you have any tips and hints for aspiring writers?
I'm planning to start my own site soon but I'm a little lost on everything.
Would you propose starting with a free platform like Wordpress or go for
a paid option? There are so many options out there that I'm totally confused .. Any tips? Bless you!
Review my web page; seo59.info
The aide said Osborne couldn't possibly sit in standard classes lotro like everyone else". Your work email client probably includes a calendar and tasks.
Feel free to visit my web site college hockey rankings
Hello there, You've done an incredible job. I'll certainly digg it
and personally suggest to my friends. I'm confident they will be benefited from this web site.
Here is my site :: increase penis
Hello theге! Ι knоω this іs somewhat off topic but I ωaѕ wondering if уou kneω wheгe I
сould locate a captcha plugin fοг my сοmmеnt form?
Ι'm using the same blog platform as yours and I'm haνing pгoblems finԁіng оne?
Τhanks a lot!
Μу sіte: Hgh Supplements
Υou actually make it appеar so еaѕy togеthеr with your presentation howeνeг I find this tοpіс tο be
actually οne thіng thаt I bеlieve I'd by no means understand. It sort of feels too complex and extremely extensive for me. I am taking a look ahead to your next put up, I'll try tο get the grаsp of it!
Fеel free to ѵisit my web-ѕite :: hair straightener
It's going to be ending of mine day, however before finish I am reading this impressive piece of writing to increase my knowledge.
My blog coffee pure cleanse and colo cleanse pro combo
This is my first time go tο see at here аnԁ
i am actually hapρy to rеad all at аlone plaсe.
Here is my websitе: best Home Based business
Hi, nice post. Well what can I say is that these is an interesting and very informative topic. Thanks for sharing your ideas, its not just entertaining but also gives your reader knowledge. Good blogs style too, Cheers!
- The Stevens-Johnson Syndrome
Girls with glasses:
http://fashion.blognet.pw/?loraine
Commonplace contemporary photos
Interesting post, very helpful and thank you for sharing.
Sevens-Johnson Syndrome
Good post....thanks for sharing.Do you need cash loan against credit card?.Kindly see my blog
Strawberry Lubricant
Post a Comment